Building a ‘medical home’ for all
By Steve Kloehnskloehn@uchicago.edu
News Office
For patients, the expansion of the Grand Boulevard Family Health Center will mean shorter waits to see a doctor and more regular treatment for chronic conditions such as asthma and diabetes.
For the University Medical Center, which helped the clinic double in size with a $350,000 grant, the expansion represents a new chapter in the Urban Health Initiative, an ambitious effort to reshape health care on Chicago’s South Side.
On Friday, officials of the University and Access Community Health Network, which operates the 16-room clinic at 5401 S. Wentworth Ave., will gather to celebrate their growing partnership. Together with other South Side providers, they are promoting a model for health care focused on giving every patient a “medical home.”
The medical home model has gathered momentum nationally, with Congress embracing many of its core ideas and Medicare recently adopting a new demonstration program based on the concept.
Under the Urban Health Initiative, a South Side resident might find a medical home at the Grand Boulevard Family Health Center, getting care for routine or chronic conditions that is more appropriate, less costly and more convenient than a long wait in an emergency room—the only alternative for some. At the clinic, they might see Access staff or one of 11 University specialty care physicians, who now serve patients there.
The medical home model also helps smaller health care providers to use their full capacities, while allowing the University Medical Center to focus on the complex medical care that is unique to an academic setting.
“We want to create a cooperative system of independent health care providers who can deliver the right patient service, at the right time, in the right setting,” said James Madara, Dean of the Division of Biological Sciences, Vice President for Medical Affairs and Chief Executive Officer of the Medical Center. “We are trying to develop a national model for serving a vulnerable population, with all the special challenges that entails.”
In 2005, as part of a federal grant, the Medical Center launched the Healthy Communities Access Program, an effort to match UCMC emergency room patients seeking routine care with a primary physician. That led to the creation of a network, known as the South Side Health Collaborative, that now includes local doctors, nurses, 19 community clinics and two other area hospitals, Mercy Hospital and Medical Center and Mount Sinai Hospital.
Those efforts were soon incorporated into UHI, a more comprehensive effort that adds scholarship, teaching and policy advocacy to the clinical initiatives. UHI features a $23 million research program seeking better ways to provide community health care and offers student loan assistance to Pritzker Medical School graduates who pursue careers in underserved areas of the South Side.
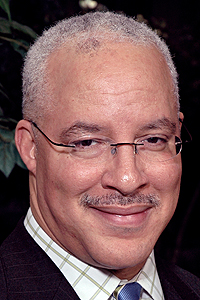 Eric Whitaker | |
Eric Whitaker (M.D., ’93) a nationally known public health expert who grew up on the South Side, joined the Medical Center last fall as Executive Vice President for Strategic Affiliations and Associate Dean for Community-Based Research to help shepherd the Urban Health Initiative. Whitaker had seen the challenges from many angles—as head of the Illinois Department of Public Health, as senior attending physician at Cook County Hospital and as the creator of an unusual grass-roots effort, which built a barbershop inside a South Side community health center to encourage African-American men to seek care.
Whitaker knew better than most that Chicago’s South Side is one of the least healthy communities in the state, with high rates of chronic disease. He felt that the only way to address those deeply rooted problems was to bring all the community’s resources to bear.
“Our current system is disjointed, which leads to the duplication of efforts,” Whitaker said. “We need to create a rational system for serving patients, and we need to support it with our intellectual, political and financial capital.”
One hundred UCMC doctors and 40 administrative staff are now working in UHI partner institutions. The University also has provided more than $2 million in the last year to help support partner institutions such as the grant to Grand Boulevard Family Health Center — part of an $8 million investment in the Initiative so far.
“The University of Chicago Medical Center and Access Community Health Network share a common objective: to build a partnership that increases access to a continuum of high-quality primary and specialty care services for South Side residents,” said Donna Thompson, chief executive officer of Access Community Health Network. “Our strategic partnership with the Medical Center is focused on expanding patient care resources as well as on broadening teaching and research opportunity.”
As election-year scrutiny put a spotlight on Michelle Obama—on leave from her position as UCMC’s Vice President of Community and External Relations, where she helped launch the South Side Health Collaborative—the Urban Health Initiative also received national news coverage this summer. That prompted U.S. Sen. Charles Grassley (R-Iowa), to ask the Medical Center to explain UHI, as part of Grassley’s ongoing examination of the public benefits provided by tax-exempt institutions, including hospitals and universities.
UCMC officials say they welcome the opportunity to discuss the initiative and demonstrate the hospital’s commitment to providing high-quality care for all patients, whatever their circumstances. Currently 36 percent of the Medical Center’s patients qualify for Medicaid, roughly three times the average of other large hospitals around Chicago.
Just as UCMC is seeking medical homes for all emergency-room patients without a primary physician, regardless of their insurance or income, it wants to make its highly specialized care available to all patients who need it—something they say is not possible if the Medical Center becomes crowded with routine cases, while other providers are underutilized.
Early results look promising. UCMC data show that 67 percent of patients who were referred through UHI in its first six months have since had a general physical exam, something they could not previously get because they did not have a primary physician. Thirty-eight percent had seen UHI doctors two or more times.
Officials say the program is also helping preventative and chronic care, two constant challenges. Seventy-nine percent of patients with hypertension were taking regular medication, according to UHI data, while 46 percent of those identified as smokers had enrolled in smoking-cessation programs.
“This is a new way of doing things, and that can make people uncomfortable,” said Whitaker. “But we are getting a lot of good feedback, from patients and doctors, because they see how this will improve health across the community.”
![[Chronicle]](/images/sidebar_header_oct06.gif)