Scans show physicians turn off empathy signal in brain to cope with pain patients experience
By William HarmsNews Office
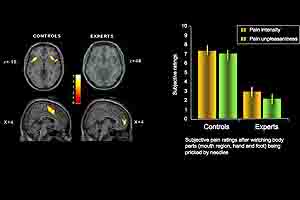 Research by Jean Decety, Professor in Psychology, and colleagues, has found that when shown pictures of people in pain, experts (physicians) do not register responses in the portion of their brain linked to empathy for pain, as did people in a control group. The physicians need to learn to control that response in order to treat patients, he said. The study also shows that the portion of the brain related to emotion regulation and cognitive control was activated in the brains of physicians when they saw the images, but not activated in the control group. | |
Physicians apparently learn to “shut off” the portion of their brain, which helps them appreciate the pain their patients experience while treating them, and instead activate a portion of the brain connected with controlling emotions, according to new research in neuroscience using brain scans.
Because doctors sometimes have to inflict pain on their patients as part of the healing process, they also must develop the ability to not be distracted or overwhelmed by the suffering, said Jean Decety, Professor in Psychology and co-author of “Expertise Modulates the Perception of Pain in Others,” published in the Tuesday, Oct. 9 issue of Current Biology and currently available online.
“They have learned through their training and practice to keep a detached perspective; without such a mechanism, performing their practice could be overwhelming or distressing, and as a consequence impair their ability to be of assistance to their patients” said Decety, who conducted the study with Yawei Cheng of the Institute of Neuroscience, National Yang-Ming University in Taipei, and other colleagues there.
Previous research, including work from Decety’s lab, has shown that the neural circuit that registers pain is activated if a person sees another person in pain. The response in this circuit, which includes the anterior insula, periaqueducal gray and anterior cingulate cortex, is automatic and may reflect a panic response developed evolutionally as a means of avoiding danger.
The research by Decety and the Taiwanese team shows for the first time that people can learn to control that automatic response.
The team performed its research in Taiwan with two groups of evenly matched men and women with a mean age of 35 and similar socio-economic and educational levels—a group of 14 physicians and 14 people with no experience in acupuncture. They were tested using a functional MRI.
Brain responses were recorded as individuals from the two groups looked at short videotape clips in which people were pricked with acupuncture needles in their mouth regions, hands and feet. They also watched as the patients were touched with Q-tips. The images appeared in random order.
Among the control group, the scan showed that the pain circuit, which is composed of the somatosensory cortex, anterior insula, periaqueducal gray and the anterior cigulate cortex, was activated when members of that group saw someone touched with a needle but not activated when the person was touched with a Q-tip.
Physicians registered no increase in activity in the portion of the brain related to pain, whether they saw an image of someone stuck with a needle or touched with a Q-tip. However, the physicians, unlike the control group, did register an increase in activity in the frontal areas of the brain—the medial and superior prefrontal cortices and the right tempororparietal junction. That is the neural circuit that is related to emotion regulation and cognitive control.
They also asked the two groups to rate the level of pain they felt people were experiencing while being pricked with needles. The control group rated the pain at about 7 points on a 10-point scale, while the physicians said the pain was probably at 3 points on that scale.
Those findings reflected the prediction the scholars had going into the study.
“It would not be adaptive if this automatic sharing mechanism for pain was not modulated by cognitive control. Think, for instance, of the situations that surgeons, dentists and nurses face in their everyday professional practices. Without some regulatory mechanism, it is very likely that medical practitioners would experience personal distress and anxiety that would interfere with their ability to heal,” the researchers write.
For Decety, this new study also casts light on the neurological mechanisms involved in empathy and empathic concern. The former relies on our capacity to share emotions and feelings with others. If there is too much of an overlap between others and self, such an overlap (reflected by similar neural circuits that automatically and unconsciously resonate between self and other) it could lead to personal distress, which is an aversive reaction. Empathic concern necessitates regulating this implicit sharing mechanism and as a consequence frees up processing capacity to act for the sake of the other.
![[Chronicle]](/images/sidebar_header_oct06.gif)