After merging resources, chemist, retina surgeon see melanin’s value in new light
By John EastonMedical Center Public Affairs
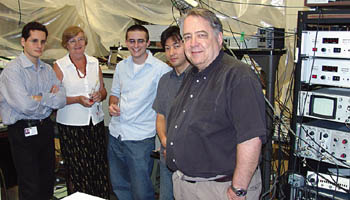 James Norris Jr., Professor in Chemistry and the College (far right), and Kourous Rezaei, Director of the Vitreoretinal Service in Ophthalmology & Visual Science were assisted by their fellow researchers Kasra Rezaei, Elzbieta Gasyna, Brandon-Luke Seagle and Yasuhiro Kobori (left to right). The team assisted Kourous Rezaei and Norris in putting together their resources to show how melanin plays a protective role within the human eye, which could help in developing ways to prevent macular degeneration. | |
Two studies from an unusual research partnership at the University have investigated a long-standing dispute about the role of melanin in the eye. The studies, one published in the Proceedings of the National Academy of Sciences and the other published in the Journal of the American Chemical Society, also suggest a new way to prevent a common cause of blindness.
James Norris Jr., Professor in Chemistry and the College, and retina surgeon Kourous Rezaei, Director of the Vitreoretinal Service in Ophthalmology & Visual Science, combined resources to show that melanin, a pigment found throughout the human body, acts like a neutralizing sponge inside cells in the retina to soak up and destroy reactive oxygen species. Reactive oxygen species, or free radicals, which are energized by light, are thought to play a major role in macular degeneration, the leading cause of blindness in people over the age of 60.
“We now have direct evidence that melanin plays an important protective role within the eye,” said Norris, a senior author of both papers. “Although melanin contains its own intrinsic free radical, we found that it absorbs a far more damaging form of free radical, converting its destructive energy into harmless heat before it can hurt the retina.”
An estimated 1.75 million Americans have decreased vision from age-related macular degeneration, or AMD, with about 200,000 new cases each year. The incidence of AMD is expected to double within the next 25 years as the number of older people continues to increase.
The disorder is far more prevalent among whites than among African-Americans. It causes gradual loss of central vision by damaging the RPE (retinal pigment epithelial) cells that lie underneath the macula, the small region of the retina responsible for fine detail at the center of the field of vision. Without RPE cells, the photoreceptors, which are the light detectors, also die. Patients lose the ability to see detail and soon they cannot read.
“This is a devastating disease,” said Rezaei. “We do not have a cure for this disease. We can only treat the secondary complications, such as growth of abnormal blood vessels. Since we don’t know how to replace or repair the dead or damaged retinal cells,” he said, “we need to find ways to protect them.”
Because people stop producing new RPE cells after birth, these cells have to last a lifetime. However, they live in a toxic environment. Oxygen concentrations at the back of the eye are very high. At the same time, the eye is constantly bombarded with light energy, which interacts with oxygen and can lead to the production of harmful free radicals—which can damage cell membranes and DNA. “It’s amazing,” noted Norris, “that the eye lasts as long as it does.”
Rezaei added, “To prevent the damage, we need to understand exactly how it happens.” He grows human RPE cells in culture in his lab, but “until now, we have had no direct way to measure the production of most dangerous free radicals. They are too small and too fast.”
Norris studies photosynthesis, in which energy from sunlight is converted into electrochemical energy, a process with many parallels to vision. To study the early steps, he uses a tool called electron paramagnetic resonance, or EPR. EPR is similar to magnetic resonance imaging, except that it measures the spin of electrons rather than of protons.
Because photochemical reactions happen extremely fast, the Norris laboratory has one of the world’s few high-speed EPR spectroscopy devices, able to record actions that occur in nanoseconds, about 1,000 times faster than standard EPR.
“Free radicals are dangerous chemicals, and dangerous chemistry takes place rapidly,” said Norris. “This lets us see some of it.”
Norris and Rezaei had another valuable asset for conducting their study: an ambitious student, interested in both chemistry and medicine, experienced with EPR and looking for a project. This was a unique opportunity for Brandon-Luke Seagle, who will begin his fourth year in the College this fall. His knowledge of chemistry and medicine enabled him to be the link between Rezaei’s cells and Norris’ techniques. He is the first author on both papers.
Using Rezaei’s cells, Norris’ technology and Seagle’s legwork, the team captured convincing and dramatic evidence that melanin protects the retinal cells. In the Proceedings of the National Academy of Sciences paper, published Wednesday, June 21, they show that increased melanin aggregation and radical migration within melanin aggregates can protect RPE cells from free-radical damage and help prevent cell death. In the Journal of the American Chemical Society paper, published Wednesday, Aug. 17, they demonstrate how melanin actually scavenges the harmful free radicals produced by high-energy blue or ultraviolet light as it flows into the eye, soaking them up and neutralizing their effects.
“We now have molecular-based evidence to support the epidemiologic data that points to the protective effects for melanin,” said Rezaei, who is testing ways to boost melanin levels, first in cells grown in culture and, if that appears promising, in animal models.
Research to Prevent Blindness, the Richter Fund and a Howard Hughes Medical Institute Undergraduate Education Initiative Grant at the University supported this project. Other University co-authors are Elzbieta Gasyna, Yasuhiro Kobori and Kasra Rezaei.
![[Chronicle]](/images/sidebar_header_oct06.gif)